Abstract
Introduction:
Kidney dysfunction is an important problem in adult recipients of allogeneic stem cell transplantation (HSCT) and independently predicts overall survival and non-relapse mortality. Kidney dysfunction occurs in ~50% of transplant recipients. More than 20% of all survivors of HSCT in long-term follow up develop chronic kidney disease. However, there is currently limited data on the cause and consequences of kidney dysfunction in adult recipients after allogeneic HSCT.
Common causes of kidney dysfunction after HSCT include chemotherapy or radiation toxicity, infections, sepsis, hepatic sinusoidal obstruction, drug toxicities due to immunosuppressive medications, thrombotic microangiopathy, as well as acute or graft versus host disease (GvHD). Kidney biopsies are seldom obtained and hence the tissue diagnosis in these patients often remains speculative. Early identification of the causes of kidney dysfunction may help define preventive and therapeutic strategies and improve outcome.
Hence, in August 2016, we designed a prospective study at our center to systematically evaluate kidney dysfunction in adult recipients of allogeneic HSCT. Herein we present our initial report of 8 kidney biopsies.
Methods:
All adult HSCT recipients with kidney dysfunction were evaluated by Nephrologists to determine the need for kidney biopsy. Kidney dysfunction was defined as either (i) acute kidney failure or (ii) proteinuria. Acute kidney failure was defined by the ' Kidney Disease: Improving Global Outcomes (KDIGO)' criteria. Proteinuria was defined as (i) spot urine albumin to creatinine ratio of ≥1 (equivalent to ≥1 g in 24 hours). Kidney biopsies were done under ultrasound guidance and the tissue specimens were interrogated by light, immunofluorescence and electron microscopy.
Results:
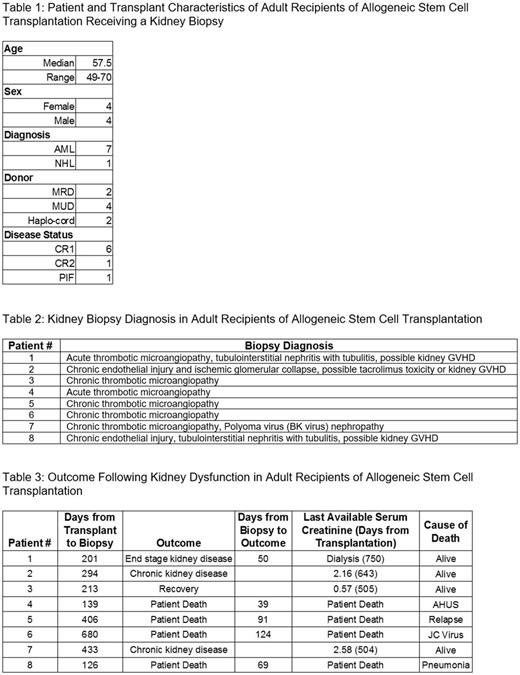
A total of 8 HSCT recipients (including one patient who had a biopsy prior to Aug 2016) underwent kidney biopsies. The patient and transplant characteristics are summarized in Table 1.
Seven of the 8 pts had AML. One patient had NHL in CR2. Four patients received a MUD transplant. Two received MRD transplants. Two received combined haploidentical and single unit cord blood transplant (haplo-cord). Six of the 8 patients received conditioning with fludarabine and melphalan. One patient received additional 400 Gy TBI. One patient received additional azacytidine.
Median time to neutrophil engraftment was 13.5 days (range 9-20). Median time to platelet engraftment was 19 days (range 14-76). There were no cases of graft failure. All patients also demonstrated either acute or chronic GvHD of other organs - most commonly skin.
All kidney biopsies were performed without complications. Kidney biopsies were done at median 254 days after transplantation (range 126-680). Baseline serum creatinine (mg/dL) prior to transplant was 0.95 (median, range 0.65-1.1, reference range: 0.64-1.27 mg/dL). Creatinine at time of biopsy: 3.0 (median, range 1.53-5.07). Urine albumin/creatinine ratio: 832 (median, range 55-2864, reference range: <30).
The kidney biopsy findings are summarized in Table 2. All patients had evidence of endothelial cell injury, either acute or chronic. Three patients had features suggestive of GvHD of the kidney while one patient had BK virus nephropathy.
Four of the 8 recipients died; 80 days (median, range 39-124) from the biopsy, 346 days (median, range 178-804) from transplantation. The clinical outcome is summarized in Table 3.
Conclusions:
Kidney biopsies post-transplant are an important diagnostic tool that should be considered for prolonged kidney dysfunction or proteinuria, particularly in the setting of other post-transplant complications. Our single-center biopsy results highlight the under-recognition of kidney dysfunction complications and complexities observed post-transplant. All kidney biopsies performed were instrumental in treatment planning. Further investigation is needed to define criteria for diagnosis and to understand the pathophysiology. This requires multi-disciplinary engagement as well as a proactive approach for obtaining kidney biopsies. With appropriate transfusion support, percutaneous kidney biopsies were performed safely without complication.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal